
Host factors and early treatments to restrict paediatric HIV infection and early disease progression
| Author List |
|---|
| Ketty Gianesen |
| Raffaella Petrara |
| Riccardo Freguja |
| et al. |
Abstract
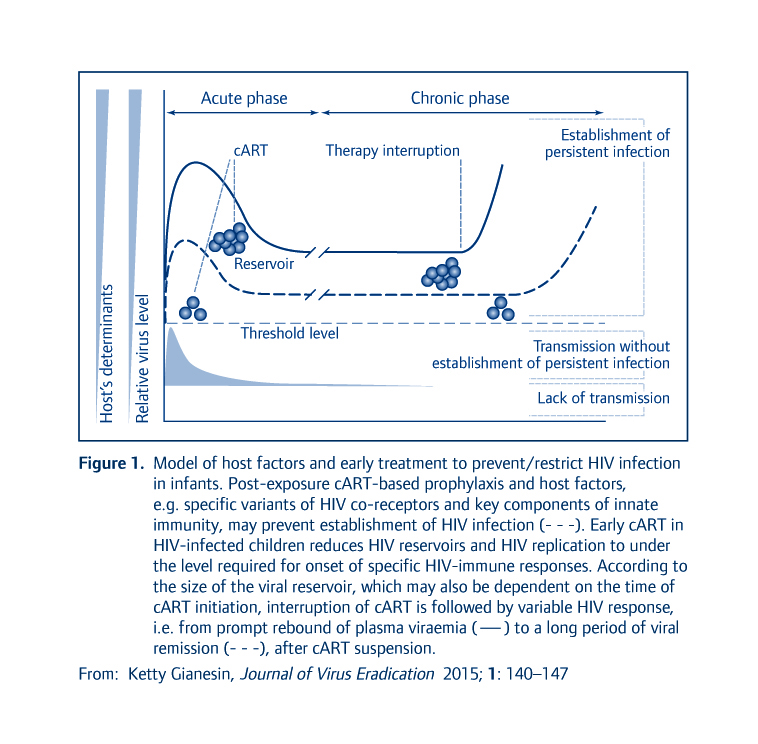
A body of evidence indicates that a threshold level of the virus is required to establish systemic and persistent HIV infection in the host and that this level depends on virus–host interactions. Mother-to-child transmission (MTCT) of HIV is the main source of paediatric HIV infection and occurs when the host’s immune system is still developing. Thus, innate resistance and immunity, rather than adaptive immune response, may be the main drivers in restricting the establishment of HIV reservoirs and the long-lived persistence of HIV infection in infants. Genetic variations in HIV co-receptors and their ligands, as well as in Toll-like receptors and defensins, key elements of innate immunity, have been demonstrated to influence the risk of perinatal HIV infection and disease progression in HIV-infected infants. Early treatments with combined antiretroviral therapy (cART) restrict paediatric infection by reducing the level of the transmitted/infecting virus to below the threshold required for the onset of immune response to the virus and also significantly reduce HIV reservoirs. However, despite long periods with no signs and symptoms of HIV infection, all early cART-treated children who later discontinued cART had a rebound of HIV, except for one case in whom a period of viral remission occurred. Which parameters predict viral remission or viral rebound after cART discontinuation? Could early cART prevent rather than just reduce the establishment of viral reservoirs ? And, if so, how? Answers to these questions are also important in order to optimise the use of early cART in infants at high risk of HIV infection.
Published
Article Category
HIV cure research
Article Type
Reviews
Posted Date
11-06-2015
| File Name |
|---|
| 1435696625JVE 1-3 Gianesin et al.pdf |
Tables & Figures
| File Name |
|---|
 [email protected] |
 [email protected] |